Understanding Injury Timelines: What to Expect from Common Musculoskeletal Conditions
- Nick Fulco

- Jun 15, 2025
- 4 min read
Updated: Jun 20, 2025
When injuries occur, one of the first questions athletes and active individuals ask is: “How long until I’m back?”
The answer depends on many factors—tissue type, severity, and the body’s natural healing capacity. At Fulco & Hall Performance & Therapy (FHPT), we believe that educating patients leads to better outcomes, clearer expectations, and safer returns to sport.
Here’s a breakdown of typical healing timelines for some of the most common injuries we treat—along with why they take time.

injury Timelines by Tissue Type
1. Muscle Strains
Muscles have rich blood supply, which supports healing, but they’re also prone to scar tissue formation that can limit flexibility or strength if not managed properly.
Grade I (mild strain): 1–3 weeks
Grade II (moderate tear): 3–8 weeks
Grade III (full rupture, often surgical): 3–6 months¹
Why it takes time: Even small tears disrupt muscle fiber alignment. Healing involves inflammation, regeneration, and remodeling. Controlled loading helps restore tissue quality without increasing re-injury risk.

2. Tendinopathies
Tendons connect muscle to bone and have less blood flow than muscle tissue, making recovery slower. Overuse often causes microscopic damage that accumulates over time.
Reactive tendinopathy: 3–6 weeks
Degenerative tendinopathy: 3–6+ months²
Why it takes time: Chronic tendon issues require tissue remodeling, not just rest. Healing involves collagen reorganization, strength rebuilding, and restoring load capacity—processes that take time and consistency.

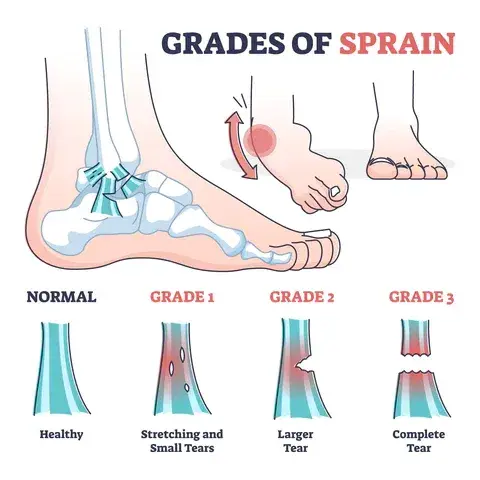
3. Ligament Sprains
Ligaments provide joint stability and heal slowly due to low vascularity. They also require neuromuscular retraining to restore proprioception and prevent instability.
Grade I (mild): 2–4 weeks
Grade II (moderate): 4–8 weeks
Grade III (complete): 3–6 months or longer³
Why it takes time: Ligaments must regain tensile strength while surrounding muscles reestablish control and balance. Returning too soon can lead to chronic instability or repeat sprains.
Surgical Recovery Timelines
Rotator Cuff Repair
This procedure reattaches torn shoulder tendons to bone using sutures or anchors. The tendon-bone interface must biologically heal, which is inherently slow.
Return to daily activity: 6–12 weeks
Return to overhead sport: 4–6 months (9+ for throwing athletes)⁴
Why it takes time: Tendon-bone healing is biologically slow, and early motion risks re-tear. Gradual strengthening is required to protect the repair while regaining functional movement.

ACL Reconstruction
The ACL is reconstructed using a graft (from hamstring, patellar tendon, or allograft), which must integrate and mature inside the knee joint.
Jogging: ~3–4 months
Non-contact sport: ~6 months
Full sport: 9–12 months⁵
Why it takes time: The graft must revascularize and remodel to match the strength of the original ligament. Surrounding strength, symmetry, and control must also be restored to prevent reinjury.

Meniscus Surgery
The meniscus cushions and stabilizes the knee. Healing depends on the procedure (trim vs. repair) and blood supply, which is limited in much of the tissue.
Meniscectomy (trim): 4–6 weeks
Meniscus repair: 3–6 months⁶
Why it takes time: Repairs require biological healing at the suture site. Early motion and weight-bearing can compromise the repair if not timed correctly.

Achilles Tendon Rupture
This major tendon stores and transfers force during walking and running. Whether surgically repaired or not, it takes extensive time to regain stiffness, strength, and control.
Walking without boot: 6–8 weeks
Jogging: ~4–6 months
Full sport: 9–12 months⁷
Why it takes time: The Achilles takes massive loads during every step. Rebuilding its ability to absorb and generate force without tearing again is a long and carefully monitored process.

Hip Labrum Repair
This surgery addresses labral tears often caused by FAI (femoroacetabular impingement), usually via arthroscopy.
Walking without crutches: 2–6 weeks
Light activity: 8–12 weeks
Full sport: 4–6+ months depending on sport demands⁹
Why it takes time: The labrum plays a key role in hip joint stability. Healing requires protection from early stress, followed by progressive mobility, control, and force absorption training.

Tommy John Surgery (UCL Reconstruction)
Common in baseball pitchers, this procedure replaces the torn elbow ligament with a tendon graft.
Throwing progression starts: ~4 months
Bullpen pitching: ~9 months
Return to competitive throwing: 12–18 months⁸
Why it takes time: The graft must anchor into bone and tolerate extreme valgus stress from throwing. The kinetic chain must also be retrained for efficient force transfer and to protect the elbow.

How FHPT Safely Expedites Recovery Timelines
At FHPT, we understand that healing is not just about time—it’s about optimizing every phase of recovery through science, communication, and individualized care. Our team uses evidence-based, criteria-driven protocols tailored to each injury and athlete, progressing clients based on strength, movement quality, and function—not the calendar alone.
We maintain strong communication with surgeons to align rehab plans with surgical techniques and timelines, ensuring consistency across the care team. We also educate clients on how nutrition and supplementation—like protein intake, collagen timing, and anti-inflammatory nutrients—support tissue healing from the inside out. Our holistic approach addresses not just the injury, but the full kinetic chain, correcting movement patterns and building strength to reduce reinjury risk.
We support the psychological side of rehab as well, helping athletes navigate fear, track progress, and build confidence. This full-circle model helps our clients safely return faster—stronger, more resilient, and better prepared than before.

References
Järvinen TA, et al. Muscle injuries: biology and treatment. Am J Sports Med. 2005;33(5):745-764.
Cook JL, Purdam CR. Is tendon pathology a continuum? Br J Sports Med. 2009;43(6):409-416.
Woo SL, et al. Healing and repair of ligament injuries in the knee. J Biomech. 2000;33(3):335-344.
Kuhn JE. Exercise in the treatment of rotator cuff impingement. Am J Sports Med. 2009;37(4):828-836.
Grindem H, et al. Return to sport after ACL injury: performance-based criteria. Br J Sports Med. 2016;50(8):505-510.
Beaufils P, et al. Management of traumatic meniscal tears. Orthop Traumatol Surg Res. 2009;95(8 Suppl):S377-S382.
Suchak AA, et al. Recovery following Achilles tendon rupture: a prospective randomized trial. J Bone Joint Surg Am. 2006;88(9):2026-2031.
Shaw G, et al. Vitamin C–enriched gelatin supplementation before intermittent activity augments collagen synthesis. Am J Clin Nutr. 2017;105(1):136-143.
Erickson BJ, et al. Performance and return to sport after Tommy John surgery among major league baseball pitchers. Am J Sports Med. 2014;42(6):1323-1332.
Grzybowski JS, et al. Rehabilitation and return to sport after hip arthroscopy. J Am Acad Orthop Surg. 2017;25(5):359-367.
Disclaimer
All FHPT blog and article material is intended for educational purposes only. The content provided is based on general information and is within the scope of practice of physical therapists in the state of Louisiana. It should not be interpreted as medical advice, diagnosis, or treatment recommendations. Individual results may vary, and the information shared is not intended to substitute for professional medical consultation, diagnosis, or treatment. Before making any decisions regarding your health, wellness, or treatment, it is essential to consult with a qualified healthcare provider. Fulco & Hall Performance & Therapy (FHPT) assumes no responsibility or liability for any outcomes resulting from the use or application of the information provided.




Comments